Huge advances in the treatment of children with cancer in Hungary: the majority now have a good chance of recovering
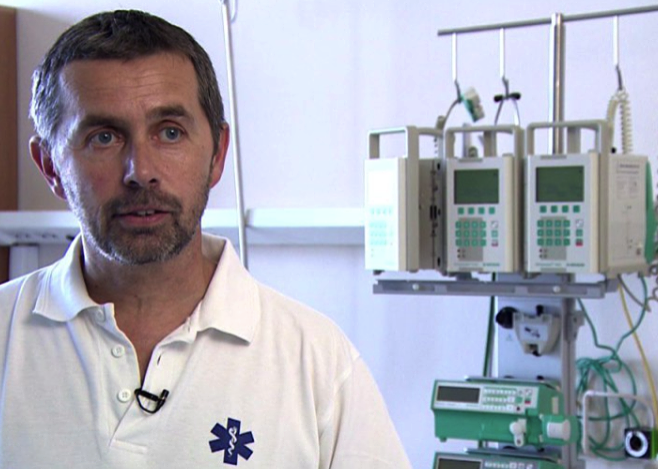
EnglishBarely half a century ago, only a small percentage of children with cancer reached adulthood, but today the situation is just the opposite: the majority recover from the disease. In addition to the continuous development of modern diagnostic and therapeutic opportunities, the establishment of paediatric oncology centres also plays an important role in this. We talked to Gergely Kriván, president of the Hungarian Paediatric Oncology Network.
How common is cancer among children?
On average, we diagnose about 250 new cases a year, but because treatments typically go on for two years, and because there is a five-year follow-up period when we regularly monitor those who no longer need active treatment, altogether we are talking about 1,000 to 2,000 children with cancer.
It is common for adults to see a doctor when it’s already too late, but children are probably much more closely monitored by parents.
That's right, neglected tumours are much rarer here, advanced cancer is almost exclusively diagnosed in adolescents, who can already hide their symptoms. Parents usually take their young children to the doctor even with minor symptoms, unnecessarily at best, but primary care for children is also effective: colleagues much rather refer the child to an oncology centre, where fortunately the suspected diagnosis often does not prove to be right.
Which are the most common types of tumour in children, and what is the difference between adults and children in this respect?
In childhood, hematopoietic tumours, especially acute lymphoid leukaemia, are the first.
The second most common are cancers of the central nervous system, but in children these are also different in location and histological type from those in adults. Neuroblastoma, i.e. tumour of the sympathetic nervous system is quite common, and various malignant lesions in soft tissue, the kidney or the bones also occur relatively often. Many oncological conditions very rarely or never occur in children, such as genital tumours and lung, gastrointestinal, or bladder cancer, which are closely related to lifestyle. With these types of cancer, in most cases the disease needs several years or decades to develop.
The development of cancer is usually explained by genetic and/or lifestyle causes, but since the latter can be ruled out in young children, are there predominantly inherited predisposing factors in the background of cancerous lesions?
Yes, and in some cases they can be uncovered, in other cases they remain hidden,
but if the disease develops very early, there is almost certainly genetic factors behind it.
This can be more and more frequently uncovered with new screening methods such as molecular genetic diagnostics, which helps find so-called mutated oncogenes that may be responsible for the development of tumours. Most of the mutations are acquired and cannot be inherited, but there are also a small number of inherited, so-called germline mutations.
Are these procedures used in all cases? After all, information on the presence of a gene that predisposes to cancer can even be life-saving in case of siblings.
We always use it in leukaemia, because in the presence of certain genetic changes, a bone marrow transplant is required even if the patient initially responds well to medication. Molecular genetic testing is also warranted in patients who relapse or eventually develop a tumour in another organ. In siblings, it is not at all certain that the same mutation is present, or if it is, it does not mean that the cancer will actually develop, as it depends on many factors.
We have encountered several cases where one of the parents had the mutant gene without ever causing a problem, while it did in the child.
What proportion of children with cancer can be currently tested with this method?
Today the rate is still low, at around 10 percent, but where a genetic mutation can be identified and there is a targeted therapy for it, it is already being used as adjunct therapy to conventional chemotherapy.
Cancer treatments are becoming increasingly mutation-specific and not tumour-specific; so instead of destroying dividing cells with cytostatics, we target the specific gene that caused the cancer. In addition to its greater effectiveness, another great advantage of this method is that the patient is exposed to much less toxic harm, his blood formation is not destroyed, his germ cells are not damaged, his hair does not fall out, his liver is not damaged, i.e. the side effects are greatly reduced. And this is extremely important, because especially in case of children, we must make every effort to ensure that the treatments they receive cause as little trauma and long-term consequences for them as possible.
So can this be the future?
This is certainly the future, especially if the planned biobank is established, where previously taken samples can be preserved, retrieved and genetically compared with current histology if necessary, for example, if a tumour recurs. There are many of these in the world; we hope there will be one also in Hungary before long.
Are there any other limitations to genetic testing than those mentioned above?
These are expensive and time-consuming diagnostic procedures, so we currently have to apply for the approval of the health insurance fund in each individual case.
The applications are always handled very quickly and always judged positively, but I have to say it is an unnecessary procedure, as overall we are talking about very few children with cancer, and doctors know very well when oncogenetic tests are relevant.
It would be more convenient if we had a yearly budget at our disposal for these procedures and then we could use them as we consider them to be reasonable.
It is also important to note that genetic testing not only has financial aspects, but their evaluation also requires specialized expertise. Our genes carry a lot of mutations, but most of them are just as harmless as, for example, many variants of the coronavirus. However, we must be able to select the ones that are relevant to the tumour, just like the British or Indian variants of SARS-Cov-2 have to be distinguished from all other variants of the coronavirus.
What are the chances for recovery of children with cancer in Hungary today?
In case of acute lymphoid leukaemia, the most common tumour, the recovery rate is 83-85 percent, which can optimally go up to 90 percent based on international experience.
Unfortunately, there will always be patients who can’t be saved by medical science, but it is very important to see that fifty years ago we were only able to successfully cure about 10 percent of children with this disease. The development is therefore enormous.
Is this mainly due to the appearance of modern diagnostic methods and therapies?
Yes, and also the fact that in 1971 we concentrated all the resources needed for the diagnosis and therapy of children with cancer in eight centres - three in Budapest and four in the countryside, in hospitals and university clinics: machines, devices, procedures, medicines, and most importantly expertise. With this, the Hungarian Paediatric Oncology Network was established, which is an important pillar of Hungarian child health care to this day.
Are there enough professionals in paediatric oncology today?
No, this is also a profession that struggles with shortages.
At least 5 paediatric oncologists-haematologists would be ideally needed in each centre, however, this number is only available at Semmelweis University and the South Pest Central Hospital, elsewhere only 2 or 3 specialists are trying to cover for the substitutions and paid leave. A total of 30-40 specialists work in the wards assisted by medical students and retired doctors.
However, the shortage is even greater in case of nursing staffs; at least 5-10 specialized nurses could be hired immediately in each and every one of our centres.
Paediatric oncology care is very stressful both mentally and physically, which must be one of the reasons for the shortage.
That’s right, but everyone who stays in this profession will experience the tremendous strength that can be drawn from the fighting spirit of these children, and also from success. Here you can really feel what it’s like to be able to solve an extremely difficult problem, or what it’s really like to help.
You mentioned that the average treatment lasts for two years, which is an incredibly long time, considering the fact that it is about nothing else but examinations and treatments practically all the time. How can families cope with this situation, their children going in and out of hospital for two years?
It’s very hard for them.
Such a diagnosis is a huge blow to families not only emotionally but also financially. In most cases it’s the mother who takes the child to the doctor or for treatments, who thus has to stop working for months, which means that the family must do without her earnings for a long time. In addition, while the family revenues decline, their expenses increase because of the need to commute regularly or, for example, the need to ensure a special diet for the child.
It would be great if there was more than ad hoc help for families to count on in this unbelievably hard situation.
In addition to treatments, how can the paediatric oncology network help affected families?
We have psychologists and spiritual care workers, and that helps a lot.
In the South Pest Central Hospital, we have a centre called Demeter House with 14 apartments, where the whole family can stay during the period of the treatment.
This opportunity is mainly used by those who cannot travel regularly from the countryside to see their transplanted child, while the child cannot go out or be discharged from the ward because they still need to be under control and close supervision. Other centres also have such homes for the children to stay in during the treatments; they are mostly maintained by foundations. There has been a significant change of approach in paediatric oncology in recent decades: we are trying to shorten the time spent in institutions as much as possible. Firstly, because the hospital is a dangerous place due to infections, secondly it is mentally better for the child not to be in a hospital environment, and thirdly, there is no better nurse than the mother.
How is the availability of hospices for incurable children today?
There are more and more hospices for children, with professional staff who are in high demand; and funding for this area should be further increased. But so-called palliative care teams (caring for patients with terminal cancer) have also been set up in some places to help relieve pain, among other things. Fortunately, a lot of progress has been made in this area as well, mainly thanks to the dedication of professionals.
